
By: Laura Sánchez,
R&D Chemist
Imagine your brain as a bustling city where neurons serve as roads, highways, and communication lines, keeping everything connected and running smoothly. Now picture cracks forming in the roads, traffic jams blocking pathways, and parts of the city falling into disrepair. This is what happens in the brain during neurodegeneration, a process central to Alzheimer’s disease (AD).
Alzheimer’s, the most common neurodegenerative disorder, steals memories, disrupts decision-making, and robs individuals of their independence. But is neurodegeneration the root cause of Alzheimer’s, or just a part of a more complex puzzle? Let’s explore.
Exploring Alzheimer’s Disease and Neurodegeneration
Alzheimer’s disease (AD) is a progressive neurodegenerative disorder characterized by the deterioration and death of neuronal cells, leading to cognitive decline and memory loss. Neurodegeneration is the primary pathological feature of this condition.
Aging is the primary risk factor for most neurodegenerative diseases, including Alzheimer’s. With aging, neurons become vulnerable, and cellular recycling processes deteriorate. This hinders the removal of damaged materials, causing accumulation in the brain. In Alzheimer’s patients, neurons release substances that activate astrocytes, brain cells that, when inflamed, contribute to brain damage.
What is Alzheimer’s Disease?
Alzheimer’s disease (AD) is a progressive neurodegenerative disorder that gradually impairs memory, cognitive abilities, and the capacity to perform daily activities. It is marked by age-related deterioration of nerve cells in the central nervous system, ultimately leading to brain atrophy.
What Happens in the Brain?
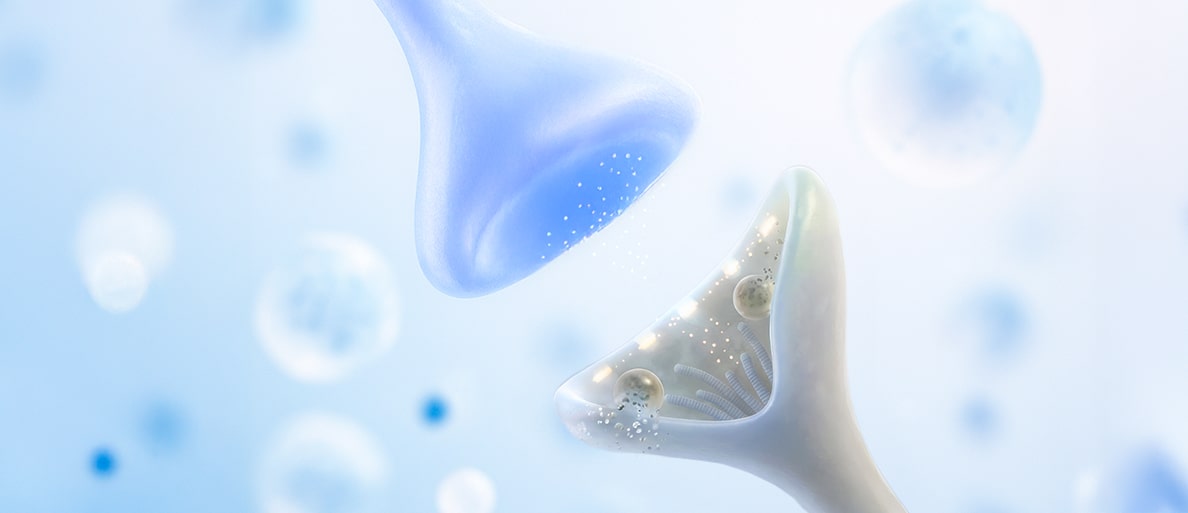
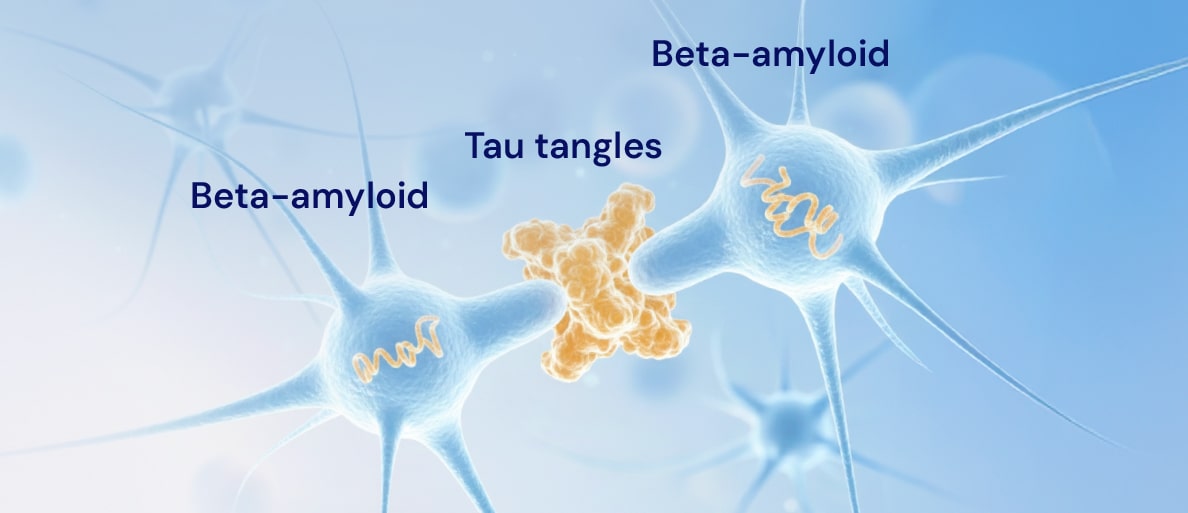
In Alzheimer’s, two harmful substances disrupt the brain’s intricate communication network: beta-amyloid plaques and tau protein tangles.
- Beta-amyloid plaques: Is the main component of neuritic plaques in AD, and its accumulation has been considered as the molecular driver of Alzheimer’s pathogenesis and progression. These plaques are sticky protein fragments that accumulate between neurons, forming clumps that block signals. Think of these plaques as roadblocks on highways, preventing information from reaching its destination. This is why these plaques are considered one of the main reasons behind the onset and progression of Alzheimer’s.
- Tau protein tangles: Inside brain cells, tau proteins normally help stabilize the internal structure, much like tracks that guide a train. In Alzheimer’s, these proteins become twisted and tangled, like a pile-up on a train track, disrupting the cell’s ability to transport essential nutrients and signals. This internal chaos eventually leads to cell death. This process is a major reason why Alzheimer’s and similar diseases lead to memory loss and other symptoms of dementia.
These processes damage neurons and trigger neuroinflammation, further exacerbating the harm. The primary risk factor for AD is advanced age, alongside genetics, as carrying certain genes like APOE ε4 increases the likelihood of developing the disease.
Symptoms of Alzheimer’s Disease
Alzheimer’s symptoms often begin subtly but progress over time. Common signs include:
- Memory loss: Forgetting recent events or familiar information.
- Executive function difficulties: Problems with planning, organizing, and decision-making.
- Visual-spatial challenges: Difficulty navigating or recognizing places.
- Language disorders: Trouble finding words or forming coherent sentences.
- Psychological changes: Alterations in personality, behavior, or mood.
Additional symptoms may include sleep disorders, autonomic dysfunction, and sensory issues like changes in smell, hearing, or vision.
Alzheimer’s affects nearly 7 million people in the U.S., and this number is expected to triple by 2050. The lifetime cost of caring for a person with AD can exceed $400,000.
The Role of Neurodegeneration in Alzheimer’s
Neurodegeneration is a hallmark of Alzheimer’s, driven by several interconnected mechanisms. Brain inflammation, known as neuroinflammation, plays a critical role in disease progression. During this process, cells like microglia and astrocytes, which typically protect the brain, can turn neurotoxic. Prolonged reactivity of these cells promotes chronic inflammation, accelerating neuronal degeneration.
Recent studies highlight the role of tau protein, whose pathological accumulations precede neuronal death and strongly correlate with cognitive decline in AD. While beta-amyloid deposits are also present, tau accumulation appears to be the key driver of cognitive dysfunction. Mechanisms such as necroptosis (a form of regulated cell death) have been identified as potential triggers of neuronal degeneration, particularly in brain areas vulnerable to AD, like the hippocampus.
Aging, another key factor, impairs neuronal homeostasis. Cellular senescence (when cells stop dividing but don’t die) exacerbates cognitive dysfunction in neurodegenerative diseases. A decline in autophagy (the cellular process that clears waste) worsens the accumulation of toxic proteins like tau, perpetuating neuroinflammation and neuronal death.
The relationship between neurodegeneration and Alzheimer’s involves more than pathological protein buildup. Chronic neuroinflammation and metabolic dysfunction are critical factors driving disease progression. Understanding these mechanisms could pave the way for new therapeutic approaches.

Can We Protect Against Neurodegeneration?
While there is no cure for Alzheimer’s, several lifestyle factors can help reduce neuroinflammation and promote brain health:
- Physical Activity: Moderate exercise reduces brain inflammation, improves brain function, and promotes neurogenesis, helping prevent damage and memory loss in conditions like Alzheimer’s. It also fosters a healthy gut microbiome, reducing overall and brain-specific inflammation.
- Gut-Brain Axis: The connection between the gut and brain suggests neuroinflammation could originate in the gut. Maintaining a healthy microbiome through a proper diet, including probiotics and caffeine, may help reduce brain inflammation.
- Quality Sleep: Sleep deprivation increases inflammatory substances and activates brain cells that contribute to neuroinflammation. Good sleep reduces these effects and helps prevent the worsening of brain disorders.
- Cannabinoids: Cannabidiol (CBD) has anti-inflammatory properties that may be beneficial for neurodegenerative diseases. It interacts with receptors in the central nervous system, reducing inflammation and protecting the brain, though more clinical studies are needed to confirm its efficacy.
How IGC Pharma is Making a Difference
IGC Pharma is at the forefront of Alzheimer’s research, focusing on innovative treatments targeting neurodegeneration and inflammation. Our work focuses on two key areas: reducing agitation symptoms in patients with moderate to advanced Alzheimer’s, improving their quality of life, and developing drugs with potential anti-inflammatory and neuroprotective effects. These medications aim not only to alleviate existing symptoms but also to slow the progression of the disease by targeting brain inflammation, a key factor in Alzheimer’s progression.
Conclusion: The Interplay of Neurodegeneration and Alzheimer’s
Is Alzheimer’s caused by neurodegeneration? While neurodegeneration and Alzheimer’s are deeply connected, as the progressive damage to neurons is the main driver of this disease, it is part of a broader network of processes. Factors such as the buildup of beta-amyloid plaques, tau protein tangles, and brain inflammation contribute to the loss of communication between nerve cells, leading to cognitive and functional decline. Understanding Alzheimer’s processes helps unravel its mysteries and opens doors to effective treatments and prevention strategies, improving life quality for those affected and their families.
The fight against Alzheimer’s requires innovation and collaboration. Through lifestyle changes and ongoing research, including IGC Pharma’s groundbreaking efforts, we can work toward reducing the impact of this disease. Together, we can protect our loved ones and preserve the memories that make us who we are.
- Andrade LJO, de Oliveira LM, Bittencourt AMV, Lourenço LGC, de Oliveira GCM. Brain insulin resistance and Alzheimer’s disease: a systematic review. Dement Neuropsychol. 2024 Feb 9;18:e20230032. doi: 10.1590/1980-5764-DN-2023-0032. PMID: 38425702; PMCID: PMC10901561.
- Balusu S, De Strooper B. The necroptosis cell death pathway drives neurodegeneration in Alzheimer’s disease. Acta Neuropathol. 2024 Jun 9;147(1):96. doi: 10.1007/s00401-024-02747-5. PMID: 38852117; PMCID: PMC11162975.
- Botella Lucena P, Heneka MT. Inflammatory aspects of Alzheimer’s disease. Acta Neuropathol. 2024 Aug 28;148(1):31. doi: 10.1007/s00401-024-02790-2. PMID: 39196440.
- Kip E, Parr-Brownlie LC. Healthy lifestyles and wellbeing reduce neuroinflammation and prevent neurodegenerative and psychiatric disorders. Front Neurosci. 2023 Feb 15;17:1092537. doi: 10.3389/fnins.2023.1092537. PMID: 36875655; PMCID: PMC9975355.
- Palmer JE, Wilson N, Son SM, Obrocki P, Wrobel L, Rob M, Takla M, Korolchuk VI, Rubinsztein DC. Autophagy, aging, and age-related neurodegeneration. Neuron. 2025 Jan 8;113(1):29-48. doi: 10.1016/j.neuron.2024.09.015. Epub 2024 Oct 14. PMID: 39406236.
- Yang C, Liu G, Chen X, Le W. Cerebellum in Alzheimer’s disease and other neurodegenerative diseases: an emerging research frontier. MedComm (2020). 2024 Jul 13;5(7):e638. doi: 10.1002/mco2.638. PMID: 39006764; PMCID: PMC11245631.





